Projects
CLIIR projects will:
- Use the EHR audit log or other EHR metadata.
- Address applied informatics research questions and assess how people interact with digital technologies, including how to use the EHR to identify socio-technical dimensions such as team structures and experience, clinician and patient behavior, etc.
- Examine clinical informatics tools deployed in care delivery settings.
Who leads CLIIR Projects? What is the process for becoming a CLIIR Project?
Any investigator at UCSF can affiliate their project with CLIIR as long as they meet the criteria outlined above. CLIIR projects will be those that engage with and benefit from the branding and expertise capabilities described above. That is, investigators can link projects to CLIIR at several steps in the process, including early- (e.g., requests for expertise on grant submissions or early-stage research projects), mid- (e.g., co-authorship or data expertise on projects already underway), or late- (e.g., present a finished project at NRN, share a project for social media dissemination) stage efforts. While we expect that much of this will happen naturally (e.g., a faculty member reaches out to one for expertise in audit log data for a project), the Director of CLIIR will have discretion to oversee and modify the CLIIR project portfolio.
Examples of Past CLIIR Projects:
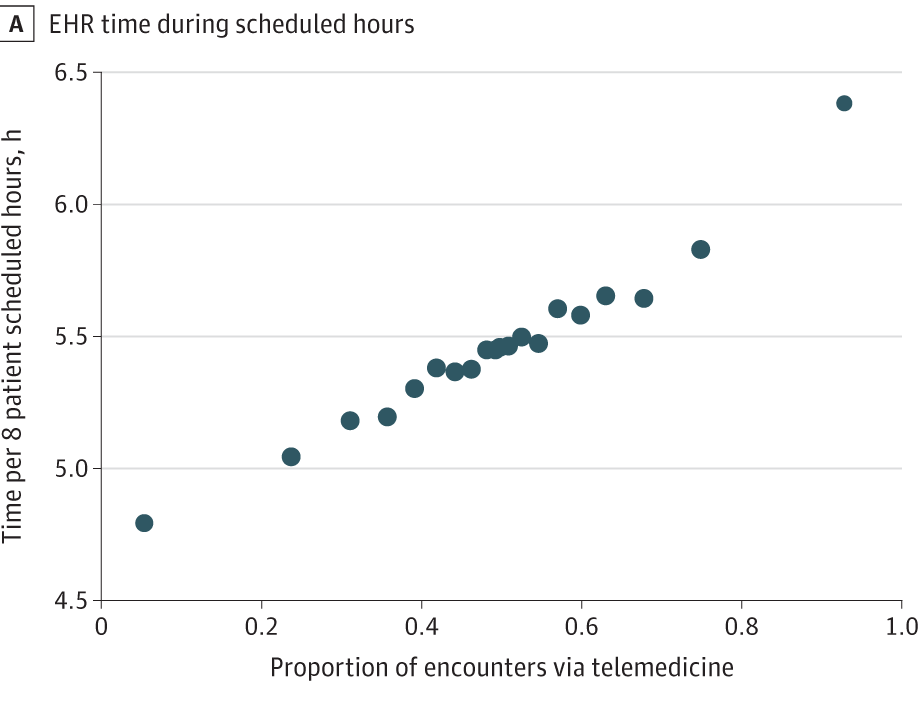
Holmgren, A. J., Thombley, R., Sinsky, C., & Adler-Milstein, J. (2023) Changes in Physician Electronic Health Record Use With the Expansion of Telemedicine. JAMA Internal Medicine.
This study uses detailed audit log data extracted from Epic's Clarity database at UCSF Health to examine how ambulatory physician EHR time varies by their use of telemedicine to deliver virtual care.
Using a two-way fixed effects multi-variable regression, this study finds greater telemedicine use was associated with greater EHR time overall, EHR documentation time, and EHR time after-hours. These results should inform policymakers decision-making around reimbursement as well as health system leaders scheduling and staffing practices as the US health care system charts a path towards sustainable telemedicine in the post-COVID world.
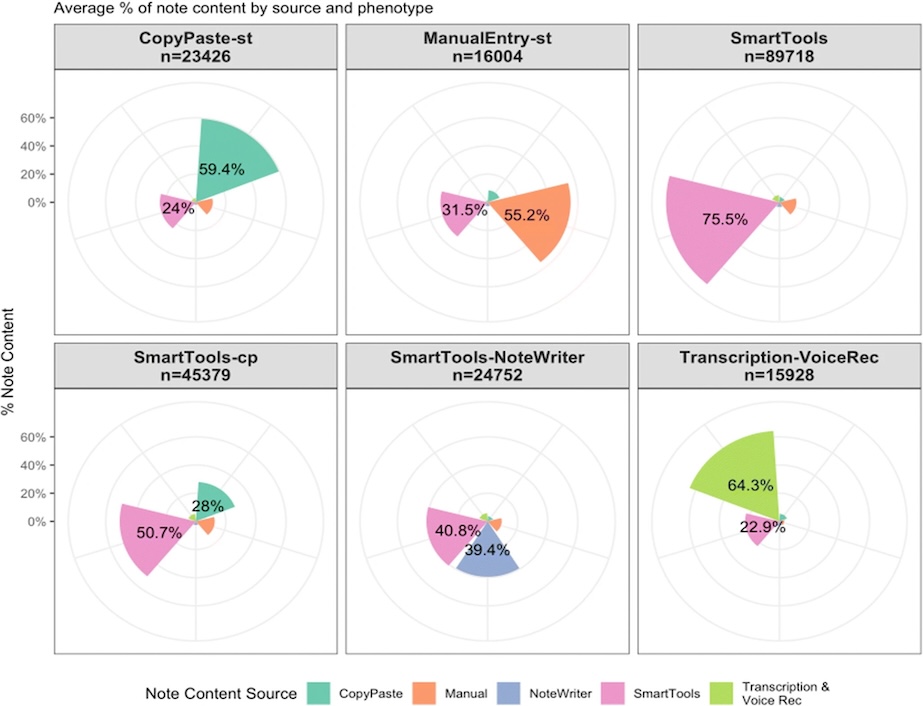
Rotenstein, L. S., Apathy, N. C., Holmgren, A. J., & Bates, D. W. (2022) Physician Note Composition Patterns and Time on the EHR Across Specialty Types: a National, Cross-sectional Study. Journal of General Internal Medicine.
This study uses national data from Epic's Signal EHR metadata tool for over 200,000 US ambulatory physicians to characterize EHR note composition strategies, how these strategies differ in time spent on notes and the EHR, and their distribution across specialty types.
Using unsupervised machine learning, this study finds 6 different "phenotypes" of physicians based on how they write notes. Physicians using primarily transcription and dictation spent less time on notes than physicians with predominant Smart Tool use, while those using mostly copy/paste spent the most time on notes. Note composition strategies have implications for time in notes and after-hours EHR use, and EHR-based documentation tools can be a key lever for institutions investing in efforts to reduce documentation burden.
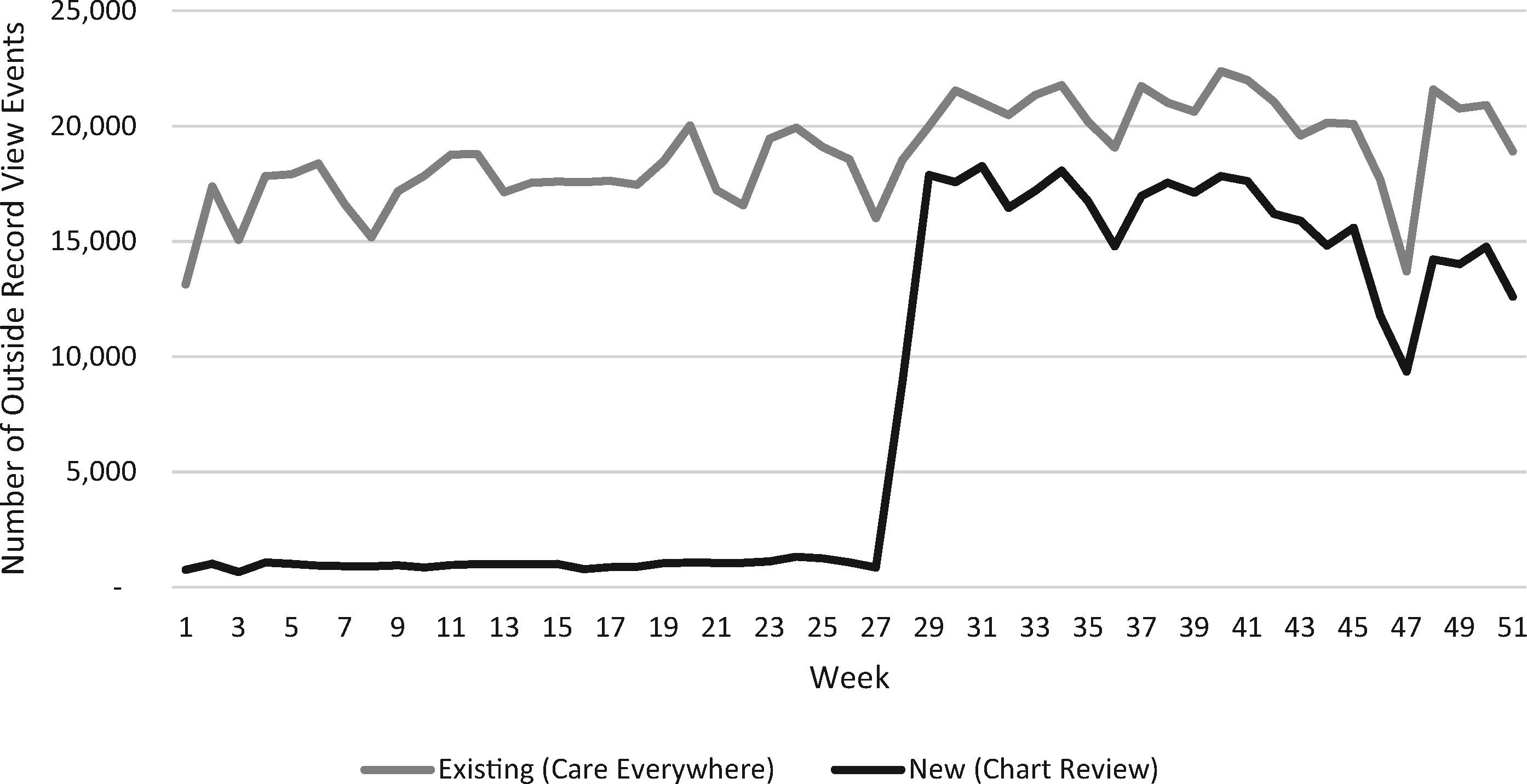
Adler-Milstein J, Wang MD. (2020) The impact of transitioning from availability of outside records within electronic health records to integration of local and outside records within electronic health records. Journal of the American Medical Informatics Association.
This study uses data from Epic's Clarity database at UCSF Health to assess whether integration between outside data and local data results in increased viewing of outside records, overall and by encounter, provider, and patient type.
Using an interrupted time series framework, there was a large increase in the level of outside record views per week. These increases were consistent for all provider and encounter types: attendings, residents, and nurses; and inpatient, emergency, and outpatient. This study highlights how user interface designs that comingle local and outside data result in higher levels of viewing and should be more broadly pursued.
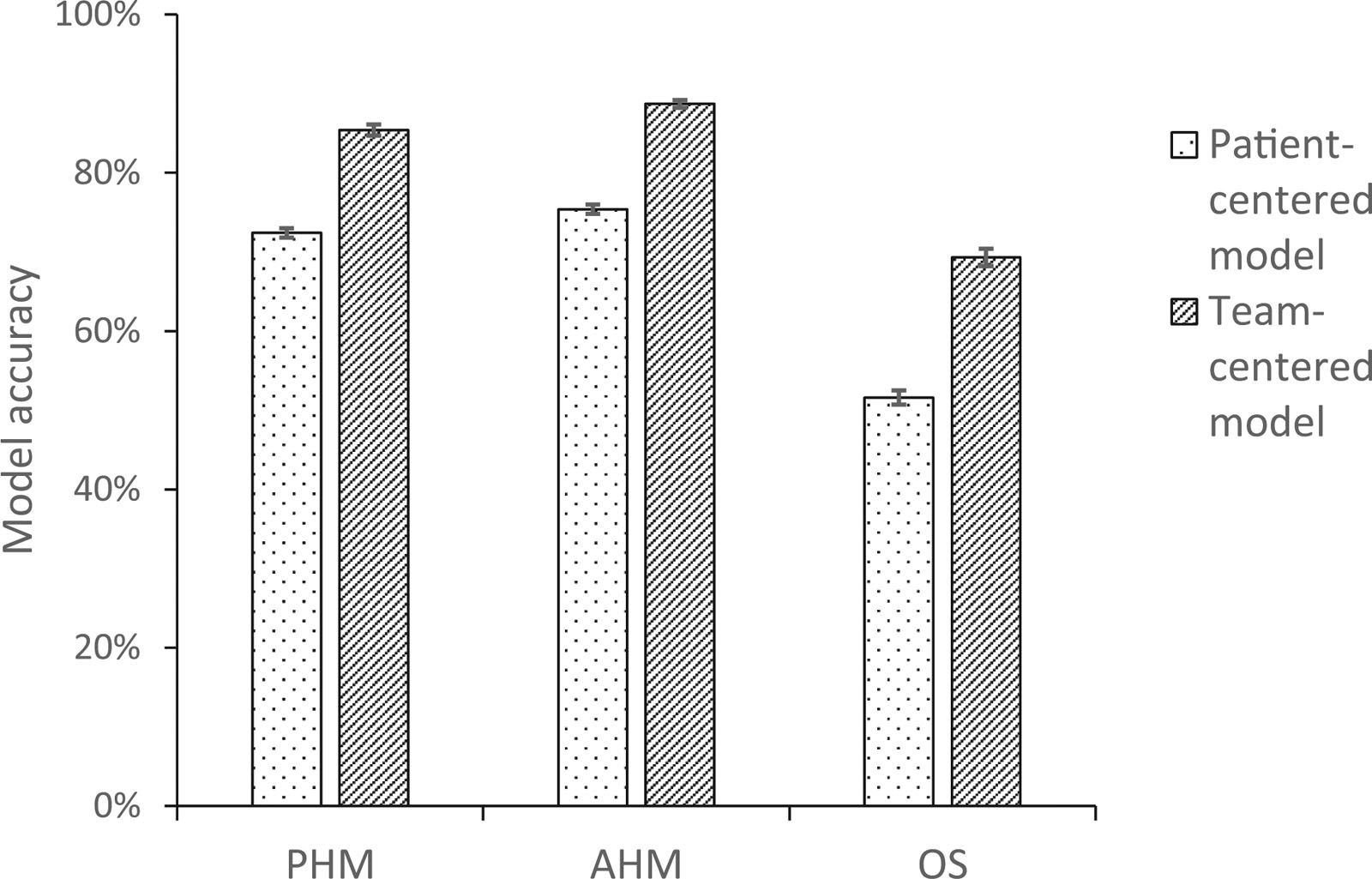
Wang MD, Rosner BI, Rosenbluth G. (2023) Where Is the Digitally Silent Provider? Development and Validation of a Team-Centered Electronic Health Record Attribution Model for Supervising Residents. Academic Medicine.
Providing trainees with data and benchmarks on their own patient populations is an Accreditation Council for Graduate Medical Education core residency requirement. Leveraging electronic health records (EHRs) for this purpose relies on correctly attributing patients to the trainees responsible for their care. EHR activity logs are useful for attributing interns to inpatients but not for attributing supervising residents, who often have no inpatient EHR usage obligations, and therefore may generate no digital "footprints" on a given patient-day from which to ascertain attribution.
This study developed and tested a novel team-centered binary logistic regression model leveraging EHR activity logs from July 1, 2018, to June 30, 2019, for pediatric hospital medicine (PHM) supervising residents at the University of California, San Francisco. These team-centered models outperformed other models acrpss 3 specialties. This study shows how EHR audit logs can be used to more accurately attribute data, enabling programs to operationalize feedback for use cases including performance measurement, case mix assessment, and postdischarge opportunities for follow-up learning.