When Primary Care Physicians See Fewer Patients, Their Workload Doesn't Shrink as Expected
New research reveals that reducing patient visits doesn't proportionally reduce EHR burden for primary care physicians
 Primary care in the US is facing a sustainability crisis. More than 40% of primary care physicians say they plan to reduce their clinical hours in the coming years, even as the nation faces a projected shortage of 70,000 primary care physicians by 2036. The pressures are mounting: growing demands for asynchronous work, such as responding to patient messages; increasing compliance requirements; and productivity targets that don't reflect how primary care has evolved in the digital age.
Primary care in the US is facing a sustainability crisis. More than 40% of primary care physicians say they plan to reduce their clinical hours in the coming years, even as the nation faces a projected shortage of 70,000 primary care physicians by 2036. The pressures are mounting: growing demands for asynchronous work, such as responding to patient messages; increasing compliance requirements; and productivity targets that don't reflect how primary care has evolved in the digital age.
One major driver of burnout among primary care physicians is the time they spend in electronic health records, particularly on tasks that happen outside of patient visits. Research has shown that physicians who spend more time in the EHR after hours and those who receive the most electronic messages are more likely to experience burnout. As a result, some physicians are intentionally limiting their clinical hours and seeing fewer patients. But does reducing visit volume actually reduce their overall workload?
A new study recently published in Health Affairs reveals the surprising insight that it’s not nearly as much as you might expect.
The research team, led by Gabe Weinreb (Harvard University), included DoC-IT’s Lisa Rotenstein and A Jay Holmgren, Nate Apathy (University of Maryland), David Bates (Brigham and Women’s Hospital and Harvard University), and Bruce Landon (Harvard University and Beth Israel Deaconess Medical Center). They analyzed national EHR data from more than 17,000 primary care physicians between 2019 and 2022, identifying 772 who experienced large, sustained reductions in their monthly patient visits.
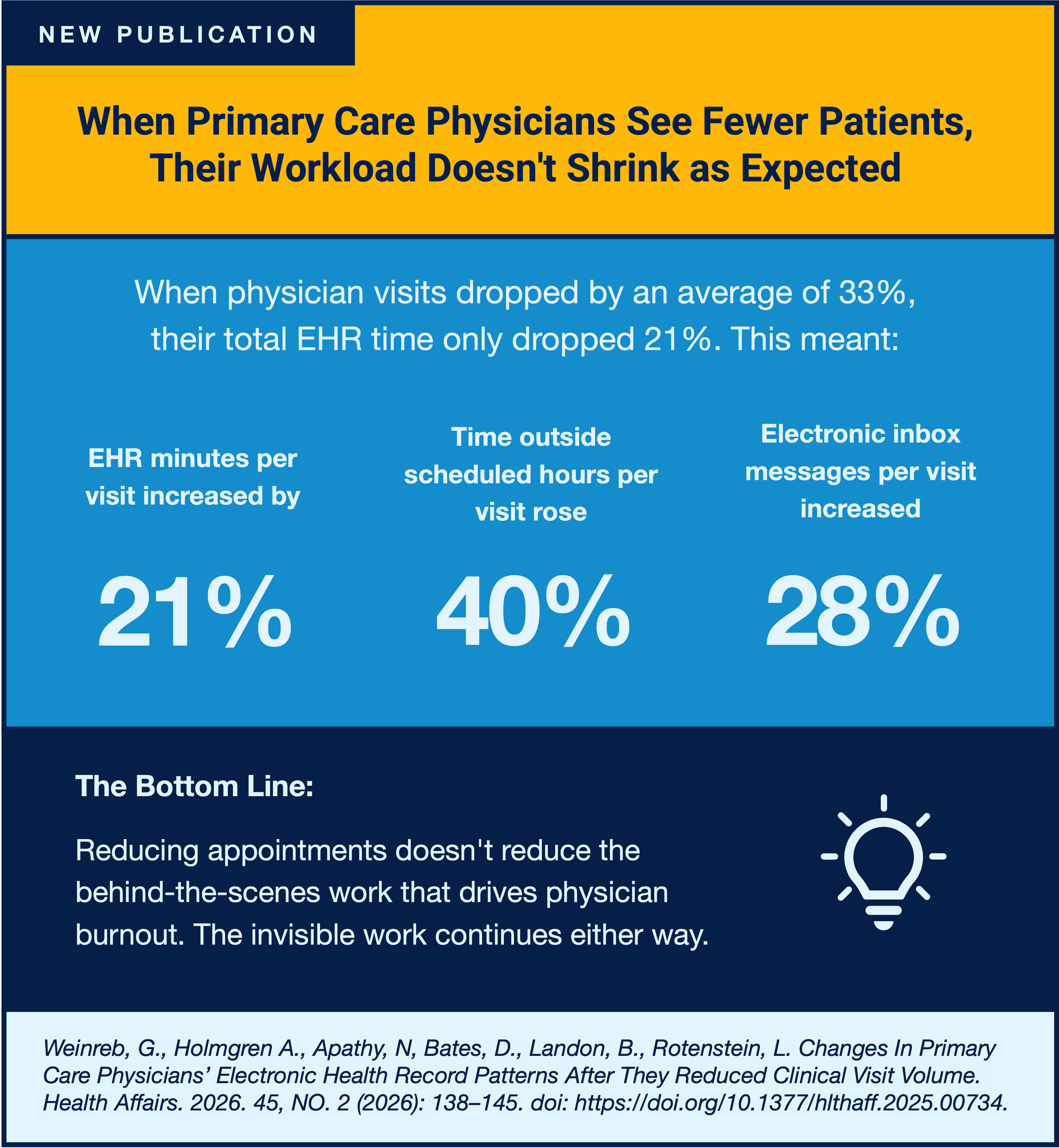
The findings revealed a striking mismatch. When physician visits dropped by an average of 33%, their total EHR time decreased by only 21%, meaning time spent in the EHR per visit actually increased by 21%. Time spent outside scheduled hours per visit rose by nearly 40%. Electronic inbox messaging per visit increased by 28%, and the patient panels became more complex, with increases in average patient age, orders per visit, and problems listed per visit.
The study points to several possible explanations. Physicians may be seeing fewer patients without actually shrinking their patient panels, which means more patients may need asynchronous care through messages instead of appointments. Some physicians might be using the extra time to provide better care to their remaining patients rather than reducing their overall workload. Others may be keeping their most complex patients, or the ones they've cared for longest, who require more follow-up work between visits.
The findings underscore a critical insight: reducing appointments doesn't reduce the behind-the-scenes work that drives physician burnout. This forces tough choices between seeing more patients, providing thorough care, and earning adequate income. The authors call for new solutions, including payment models that compensate physicians for work done outside visits, AI tools to help manage message volume, and better workflows for asynchronous care.
Simply seeing fewer patients won't solve the burnout crisis. The invisible work continues either way.
"Changes In Primary Care Physicians' Electronic Health Record Patterns After Reductions In Visit Volume”
By Gabe Weinreb (Harvard University), A Jay Holmgren (UCSF, DoC-IT), Nate Apathy (University of Maryland), David Bates (Brigham and Women’s Hospital and Harvard University), Bruce Landon (Harvard University and Beth Israel Deaconess Medical Center), and Lisa Rotenstein (UCSF, DoC-IT, and Brigham and Women’s Hospital)
This work was generously supported by the Physicians Foundation and the American Medical Association.